In order to fight pathogenic invaders like bacteria, viruses, fungi, parasitic worms, aberrant cells, etc., the immune system is made up of ...
In order to fight pathogenic invaders like bacteria, viruses, fungi, parasitic worms, aberrant cells, etc., the immune system is made up of a complex network of immune cells that collaborate with proteins like cytokines. With the exception of specific disorders like autoimmune diseases, they have a special capacity to tell self-molecules apart from non-self-molecules. Except for identical twins, each person's bodily cells have a distinct Major Histocompatibility Complex (MHC) protein on their surface, which is used to distinguish between self and non-self. MHC I and MHC II are two different types of MHC proteins that distinguish the body's own cells from foreign or pathogenic cells and display antigen on the cell surface, respectively. MHC II, however, is also present in immune cells called antigen-presenting cells (APCs), which display phagocytosed microbe on the cell surface. Red blood cells do not have MHC proteins.
Table of Contents
- Innate and Acquired Defense Systems1. First Line of Defense
2. Second Line of Defense
- Phagocytes (eating cells) and their relatives
- Mechanism of the second line of defense
3. Third Line of Defense
- Humoral or antibody-mediated immune response
- Mechanism of antibody-mediated immune response
- Cell-mediated immune response
- Mechanism of cell-mediated immune response
Innate and Acquired Defense Systems
Two forms of bodily defences exist against invaders:
The two types of reactions are acquired (adaptive/specific) and innate (natural/non-specific).
- No matter how often a pathogen is exposed, innate reactions are the same, but acquired reactions are better with each consecutive exposure to foreign particles.
- Phagocytic cells including neutrophils, monocytes, and macrophages as well as Natural Killer (NK) cells are used in innate reactions. However, antigen-specific B and T cells or antigen-presenting cells are involved in adaptive responses (APCs).
- When a foreign attack occurs, innate reactions react right away, but adaptive responses need more time to respond.
- Be a result, learned responses are referred to as particular and innate responses battle against certain sorts of invaders.
- The first and second lines of defence are part of the innate reaction, whereas the third line is part of the learned response.
- First line of defense
- Second line of defense
- Third line of defense
1. First Line of Defense
i) Physical defenses:
- Skin: The epidermis, dermis, and hypodermis are the three layers of skin. The epidermis, which is the top layer, is densely covered in keratin and dead skin cells. These defunct cells are constantly being replaced and shed. Because it is mechanically strong and very water-resistant, keratin inhibits the development of microorganisms.
- Nasal Hairs: While tiny cilia along the respiratory system whisk mucus and trap inhaled particles towards body openings where they may be expelled from the body, nasal hairs filter air tainted with bacteria, dust, and dirt.
- Mucous membranes: Mucus, a slimy material produced by the mucous membranes lining the respiratory, urinary, and reproductive systems, collects unwanted particles and guides them out of the body by mechanical processes including shedding, coughing, peristalsis, and flushing of physiological fluids (e.g. urination, tears)
ii) Chemical defenses:
- Sweat, tears, mucus, and saliva: Saliva, mucus, sweat, and tears all have pathogen-killing enzymes. Lysozyme, an enzyme present in saliva, sweat, and tears, may destroy the cell walls of bacteria and eliminate them. Similar to this, secretory IgA function by destroying peptidoglycans in bacterial cell walls. Dermcidin, cathelicidin, defensins, histatins, and bacteriocins are antimicrobial peptides (AMPs). In reaction to pathogens on the skin, AMPs are created.
- Cerumen or ear wax: The fatty acids in cerumen, or ear wax, cause a pH drop to between 3 and 5, shielding the auditory canal from external objects like germs.
- Gastric juice: Pathogens that enter the stomach through the mouth or nose are killed by the extremely acidic nature of gastric juice (pH 2-3).
- Urine: Acidic urine flow kills microorganisms and is directed out of the urethra.
- Serum: Serum (unsaturated fatty acids) is found to include certain molecules that make it easier for some microorganisms to get the nourishment they need while still reducing water loss and inhibiting microbial development.
iii) Biological defenses:
2. Second Line of Defense
Phagocytes (eating cells) and their relatives
- Basophils: These make up only 1% of WBCs. Since they emit heparin and histamine when activated, they are renowned for their inflammatory response linked to allergies and asthma.
- Mast cells: Despite being tissue-based, they have functional similarities with basophils. As a result of being activated by various inflammatory mediators and antigens, they exhibit an inflammatory response. Once it detects pathogens, it produces granules that contain inflammatory histamine.
- Monocytes: They are referred regarded as the "trash trucks" or "vacuum cleaners" of the immune system and are associated with scavenging. These make up between 2 and 6% of the WBCs in the blood. The biggest WBCs are made up of these cells. They enter tissues in response to inflammation and undergo differentiation into macrophages and dendritic cells after leaving the circulation.
- Macrophages: These are present in the tissues and organs and engulf and digest pathogens missing certain surface proteins to healthy body cells, such as malignant cells, bacteria, cellular debris, etc. They discharge a variety of compounds, including enzymes and complement proteins, as well as regulatory substances like interferons, interleukins, etc. Since these processes absorbed antigens and presented them to T cells, these active T cells and consequently the adaptive immune system by serving as "antigen-presenting cells."
- Dendritic cells: These can be distinguished from monocytes, which are found in tissues that come in touch with the outside world, such as the skin, nose, lungs, etc. Innate immunity and adaptive immunity are connected by these cells. When they locate foreign particles, they go to lymph nodes where they engage with T and B cells to deliver the antigen and start an immune response. These are referred to as dendritic in that their cellular architecture resembles a "tree-like" structure.
- Neutrophils: These make up around 65% of WBCs and are the first immune cells to react to invaders. They deliver messages to other immune cells and squeeze out through capillaries into the infection location. Therefore, they are often referred to as "patrol tissue." They have a brief life expectancy of about eight hours after being expelled from bone marrow.
- Natural Killer (NK) cells: These cytotoxic lymphocytes are the only ones in the innate immune system that may act quickly against tumour or virus-infected cells without priming or prior activation. These are most recognised for their "natural" propensity to kill, which subsequently aids in the detection and management of early cancer indications.
Mechanism of the second line of defense
3. Third Line of Defense
Humoral or antibody-mediated immune response
- Plasma B cells: These eject immunoglobulins, which are antibodies (Igs).
- Memory B cells: They provide the immune system a durable memory.
Mechanism of antibody-mediated immune response
Cell-mediated immune response
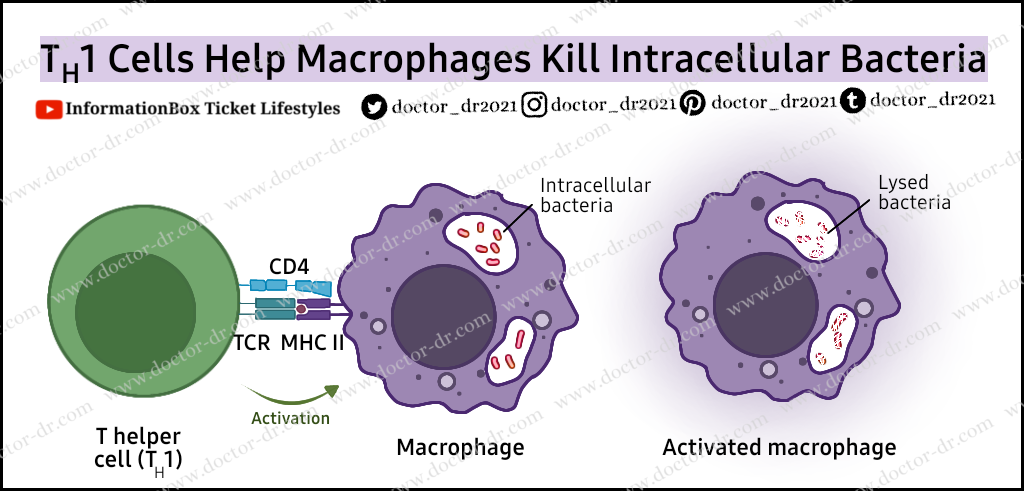
- TH /T helper cells (CD4+): These cells release cytokines that promote clonal development of TH cells, activation of macrophages to cause phagocytosis, and B cell division and maturation into plasma and memory cells.
- Tc (T- killer/cytotoxic) cells (CD8+): These cells cause the pathogen's DNA to be destroyed by secreting cytotoxin or by puncturing the membrane of the pathogen with perforin. Cell lysis or apoptosis is the effect of this.
- T-suppressor cells/Treg/Regulatory T cells: are a component of the body's self-check system that shuts down T cell-mediated immunity once the pathogen has been eliminated. They also aid in the prevention of autoimmune illnesses.
- T-memory cells: These cells don't proliferate unless they have already been exposed to an antigen. When the same antigen surfaces again, they are stimulated to differentiate into cytotoxic T cells and eradicate the infection.






ليست هناك تعليقات